%20website%20header.png) REQUEST DEMO
REQUEST DEMO
.png)
Eliminate backlogged claims with expert AR recovery services designed for healthcare providers, ensuring faster collections and higher revenue.
.png)
Unpaid claims slow down revenue, stress staff, and make it harder to run a practice. Jorie AI fixes that. Our AR recovery services get your outstanding claims cleared faster, accurately, and with minimal manual effort.
Slow or missed claims cost you money. With Jorie AI, you get AI-powered bots with expert RCM specialists to follow up on every claim, verify eligibility, correct errors, and recover revenue that often sits uncollected.
With us, practices see up to a 75% reduction in denials and significant improvements in daily payments.
See how healthcare organizations like yours have transformed their revenue cycle with Jorie AI.
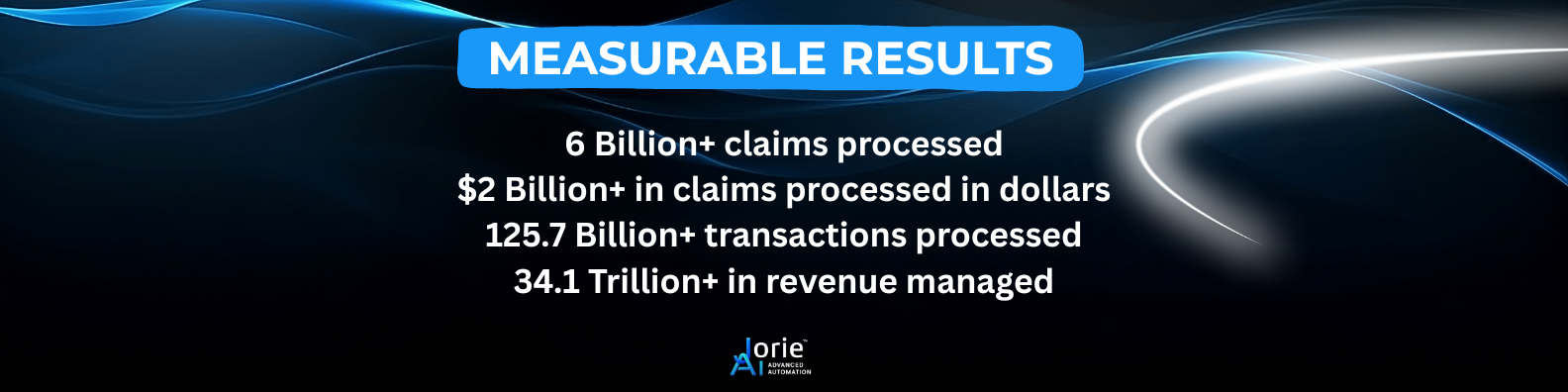
We combine technology and human expertise to deliver measurable results.
We go beyond claim follow-ups to help recover revenue, reduce errors, and keep cash flowing consistently:
Recovering accounts receivable isn’t about adding more people. It’s about being smarter by focusing on the right claims and handling them the right way.
Let’s break down our process.
Before we do anything, we first examine your current AR landscape. We look at your claims data, denial trends, and workflows, so that we can pinpoint any revenue leaks. We go deep into your processes, tech stack, and past claim outcomes to reveal the biggest gaps and opportunities for improvement.
We prioritize high-value accounts and aged claims because they have the biggest impact on your cash flow. That approach gets results faster and clears the most urgent issues first.
While our AI bots take care of repetitive tasks like eligibility checks, following up on claim status, and posting payments, our RCM experts tackle the complicated stuff like denials, underpayments, and claims that need careful human judgment.
Claims are recovered efficiently and posted automatically. You get transparent, real-time reporting that shows exactly how much revenue is being recovered and where improvements are happening, so you stay in control of your financial health.
See how the process works.
Jorie AI helps healthcare organizations of all sizes streamline revenue cycle operations, reduce denials, and recover more revenue.
We deliver results where it matters most:

Hear directly from the healthcare leaders we’ve helped, how Jorie AI streamlined their AR recovery, improved cash flow, and transformed their revenue cycle operations.
"Jorie AI’s hands-on approach and continuous support have transformed our revenue cycle, helping us optimize efficiency and drive better results."
- Gulf Coast Eye Institute McAllen, TX
AR (Accounts Receivable) Recovery Services help healthcare organizations identify, correct, and collect unpaid or underpaid claims. This includes tracking claim status, resolving denials, verifying eligibility, posting payments, and recovering underpayments.
The goal is simple: get revenue out of limbo and into your accounts quickly, accurately, and efficiently, so your practice can focus on patients instead of paperwork.
Explore tools and insights to help you optimize revenue cycle management and AR recovery:
Stop letting unpaid claims slow your practice. Partner with Jorie AI and start recovering revenue faster, reducing denials, and freeing your staff from tedious follow-ups. It only takes a few minutes to set up, and you’ll start seeing results almost immediately.
Have more questions about AR recovery? We got you!
By quickly identifying and resolving unpaid or underpaid claims, Jorie AI accelerates collections, reduces denials, and shortens AR days, so revenue reaches your accounts faster.
Clients typically see up to a 75% reduction in denials and significant improvements in first-pass claim approvals and payment turnaround times.
Recovery speed depends on claim volume and complexity, but most clients begin seeing measurable results within a few weeks.
Yes. Our AR Recovery Services cover a wide range of specialties, from primary care to complex specialty practices.
We target high-value and aged claims first to maximize immediate impact, while also addressing patterns in denials and eligibility errors to prevent future delays.
Basic AR reports, claim histories, and access to your billing system or EHR. Once we have that, our AI and RCM experts handle the rest.